The Math of salt loss

In light of the recent tragedy at Ironman Frankfurt, where a 30-year old athlete collapsed at the finish and died in hospital a few days later, there has been broad speculation that the significant heat during race day and the athlete's hydration conduct caused irreversible brain swelling.
Questions have arisen as to the likelihood of hyponatremia or over-hydration. "Swelling of the brain is the cause of death," said Professor Leo Latasch, head of the medical emergency team of the Gesundheitsamt in Frankfurt, and it was likely caused by insufficient salt intake while racing in unusually hot conditions. According to Professor Latasch, the athlete drank mostly water during the race and did not take in enough minerals.
Meanwhile, Dr. Tim Noakes tweeted, "Another avoidable death from hyponatraemia. Can't happen if athletes advised to drink to thirst, not to a schedule."
What follows was originally published here in 2009. Not specific to this case, it's a mathematical and scientific model.
The strategy for some athletes is survival — just getting to the finish line. For others, their day is a question of performance. Both groups struggle with the balance between survival and performance when it comes to proper hydration, nutrition and electrolyte balance.
There is no doubt that to participate in an 8-to-17 hour event one must take on board some calories, fluid and electrolytes to offset at least some of that which is consumed or lost during the event. For those with performance goals, the delicate balance between too much and too little can be their undoing, while for those simply trying to survive, the balance, as I will illustrate, can have much more dire consequences.
Much has been written about proper electrolyte and fluid replacement during endurance sports, however I have yet to find a comprehensive mathematical model that illustrates the full scope of struggle between consumption and replacement during the course of an endurance event or long training day.
Some ground rules: In this model I will be discussing the loss and replacement of sodium exclusively. A quartet of electrolytes play a critical role in muscle function and other biochemical processes. The loss of sodium is by far the most substantial and well-studied. The loss and replacement of potassium, calcium and magnesium follow suite, and their levels will be affected over time through sweat loss as with sodium. It is beyond the scope of this particular article to discuss the importance of their replacement except to indicate that without proper supplementation, the concentration of these critical electrolytes in blood will also decrease and can reach a level that can compromise performance, or worse.
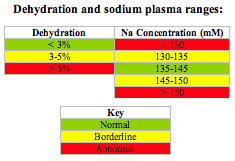
Consider that a common misconception that hyponatremia is simply due to low sodium levels in blood. In fact, hyponatremia, as defined by plasma concentration below 135 mM sodium, can exist either due to reduced levels of sodium in a normal blood volume or by normal sodium levels in an increased plasma volume as will be illustrated. Hypernatremia is defined by plasma concentration above 145 mM sodium and is also a serious medical condition, and can be caused by either increased levels of sodium in normal blood volume or normal sodium content in reduced plasma volume.
The mathematical model described below may be worth considering as it relates to the importance of your electrolyte and fluid replacement strategy.
DEHYDRATION AND HYPONATREMIA
There are 2 characteristics that will be explored and are at odds with one another. They are:
1) Dehydration: The loss of plasma volume (blood) due to sweating, urine and exhalation.
2) Electrolyte loss: Hundreds of scientific studies have found that sweat contains a significant component of sodium along with other electrolytes in lesser amounts.
In both cases, the loss of fluid and electrolytes through sweat is highly variable depending on the individual, fitness/acclimatization and temperature/humidity.
The Consumption-Loss model
One understanding necessary for athletes to accept the following mathematical model is that athletes face a losing battle on the race course.
Energy: From an energy standpoint, the caloric consumption can range anywhere from 600 to 1500 kcal/h. It has been shown through multiple studies that an average athlete can readily absorb (process) between 200-600 kcal/h. A simple glance will quickly show that racing an Ironman is a losing proposition. Luckily, we have energy stores in our bodies that can, over time, provide the deficit. This means that in theory you could finish an Ironman without eating, by relying on the 30000+ kcal stored in fat, at an aerobic pace or slower, the body has sufficient reserves to survive to the finish. From a performance perspective, athletes would be wise to replace some of the caloric loss so as to provide the engine with fuel for a higher output.
Fluid: From a standpoint of fluid loss and intake, a similar situation exists with energy, however, the operative window is much more narrow and of much greater consequence than lack of food. As the model will demonstrate, dehydration can set in rapidly. While exact conditions and the athlete will determine when dehydration will occur, it is a certainty that performance will suffer and significant medical issues should dehydration become more severe. Authorities have suggested that a minimal amount of dehydration (<2% body weight) may be tolerated without compromising performance. At 5-6% water loss (by body weight), sleepiness sets in, as well as headaches, nausea or tingling in the limbs. At 10-15% water loss, muscles can lose control, hearing may be lost, and vision may dim. Losses over 15% are usually fatal.
Electrolytes: It is one of the goals of the current article to propose a similar model for electrolyte loss and related consequences as documented for fluid loss. The body has a finite content of sodium. The bulk of active sodium ions are stored and available in blood plasma. No immediately-available repository of sodium has yet been reported discovered in any tissue or organ within the body to date. While bones and some other tissues do contain sodium, these stores have been shown not to be readily available within the timeframe under discussion (up to 10 hours). With finite stores of this mineral and a strong propensity for loss through sweat, and to a lesser extent in urine and stool, sodium is recognized as a vital nutrient in a healthy diet. While a typical Western diet over-contributes sodium, athletes can and should be forgiven for increasing their sodium intake to approach sodium losses over time. Similar to fluid and calories, a long-term deficit of sodium will be detrimental to the body. It continues to be a surprise that athletes and coaches do not recognize sodium as just another “expense” of racing, and as with fluid and energy, the finite store of our body can be taxed by unusually high losses as might occur during endurance events.
What happens during sweating? Initially, water moves from tissue to blood as sweat is lost, to keep electrolytes within normal physiological levels. Finally a breaking point is reached when the body can no longer compensate by removing water from tissue, and then plasma volume begins to decrease. As such, early on, sweat can be lost while keeping the apparent plasma concentration of electrolytes nearly constant (as evidenced by body weight loss and a constant specific gravity of urine). In other words, dehydration can occur without the usual indicators (specific gravity of urine increasing), at least initially. To maintain homeostasis, the body will make whatever adjustments necessary and possible until normal levels can no longer be maintained.
MATHEMATICAL CALCULATIONS
The following spreadsheets show several strategies of rehydration and sodium supplementation over the course of 10 hours. There are a few assumptions that must be considered that make this a simplified calculation as compared with real life or lab testing:
– Fluid loss is through sweating only. Losses from urine and transpiration are ignored.
– Electrolyte loss is through sweating only. Losses from urine and stool are ignored.
– Sweat is assumed to be lost at a constant rate and with a constant electrolyte profile over time.
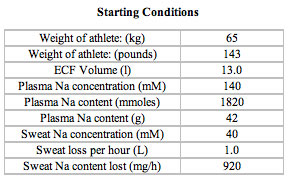
For this example, consider a typical 65 kg athlete (143 pounds) with 15 L (15 kg) of plasma of which 13 L (13 kg) is water (20% body weight). Sweat rate is set at 1 L/h (range 0.2 – 4.0 L/h). The sodium content of sweat is set at 40 mM (range 20-80 mM) meaning that 1 L of sweat would contain 920 mg of sodium.
The following table describes 3 examples of rehydration that do not involve any level of sodium supplementation. As discussed above, as the plasma volume decreases, the sodium concentration actually increases. In case study #1, after 2 hours without fluid consumption, the sodium content of blood has reach a dangerous hypernatremic level of 158 mM, however, this athlete will likely become thirsty long before this happens. Meanwhile, as shown in case #2, an athlete replacing 50% of the fluid lost (ie. 500 mL/h) will maintain plasma volume and sodium content within a normal range for 3 hours. However, long term application of this strategy clearly demonstrates that both hypernatremia and dehydration will occur. This athlete will also likely become thirsty long before a dangerous level is reached. Case #3 explores 100% fluid replacement with water (1 L/h). While this is an effective strategy to prevent dehydration, it is clear that hyponatremia begins as soon as 2 hours and at a dangerous level by 4 hours. This example demonstrates very clearly what can “go wrong” for athletes walking a marathon (4+ hours) and drinking water to replace all fluid loss. Hyponatremia will result and has caused death at events around the world for exactly this reason, called “water intoxication”.
Definitions:
mmol: millimol- an amount of material (in the case of sodium, 1 mmol = 23 mg)
mM: millimolar- concentration in mmoles per liter (so 23 mg sodium in 1 L = 1 mM)
ECF Volume: extracellular fluid- component of blood that is liquid. For an average adult, it is approximately 20% of body weight.

Now consider a combination strategy of fluid and sodium replacement. Once again, consider the same athlete losing the same amount of fluid (sweat) and sodium. In case #4, the athlete replaces 100% of the fluid loss (1 L/h) with the addition of 400 mg sodium/h. This strategy can be effective for 2 hours as well. However, over time the sodium loss exceeds that which is consumed and the plasma begins to dilute causing severe hyponatremia by 6 hours. This athlete is drinking too much, again causing “water intoxication” albeit with a slower onset due to the consumption of some sodium to replace that which is lost. Case #5 explores an example where an athlete consumes 75% of the fluid lost (750 mL/h) and takes a considerable amount of sodium (1000 mg/h) for the athlete’s size and sodium loss. In this example, the athlete maintains a reasonable level of hydration throughout 10 hours, however due to the excessive sodium consumption, severe hypernatremia will occur by 4 hours. This athlete is taking in too much salt! They will likely become very thirsty and increase their fluid consumption, which brings us to case #6. This athlete chooses to replace a reasonable 90% of their fluid loss (900 mL/h) and to supplement 700 mg sodium per hour. Based on the calculations and assumptions, this athlete has the most likely chance of avoiding dehydration, hypo- and hyper-natremia. This athlete will be the most likely to perform and not just survive.

THE REAL WORLD
How does this reconcile with real-world results? Studies have shown that electrolyte loss is real but that plasma electrolyte levels do not appear to change significantly early in exercise. In the case of sodium, plasma levels can actually rise due to loss of plasma volume (as shown in the above mathematical model). For potassium, the intracellular (within the cell) content is significantly higher than that of the plasma, and as a result transport of potassium out of cells can replace some of that which is lost in sweat. However, in both cases, upon rehydration, the final concentration of electrolytes in plasma will fall. Look no further for real-life examples than the cases of hyponatremia at Ironmans and marathons around the world on a regular basis.
Fatalities due to hyponatremia have been due to “over-hydration” where plasma volume is high and sodium content is low, defining a low plasma sodium concentration. Typical suggestions “not to overdrink” will indeed prevent this situation, however as the above mathematical model shows, the risk of performance-limiting dehydration over time is significant.
Also, it should be noted again that the assumption in the above model simplify a complex process. For example, sweating decreases as the body becomes dehydrated in order to preserve water. The body core temperature increases due to poorer cooling; however fluid loss through sweat is reduced.
Athletes trying to eat and drink to replace exactly what they are losing will also face a losing battle. Physiologically, most athletes are limited in the amount of fluid, electrolytes and energy they can effectively absorb under stress. A reasonable strategy is to replace what your body can absorb at a level as closely possible to what is lost.
SUMMARY AND RECOMMENDATIONS
Extended periods of exercise at even moderate intensity can cause significant losses of fluid through sweating. Electrolytes, including sodium, potassium, magnesium and calcium, are present in this sweat at levels that over time will cause your body to become depleted. Muscle cramping, loss of performance, heat stress and other symptoms can result from reduced electrolyte levels and dehydration. Consumption of water will act to further dilute remaining electrolyte reserves and can exacerbate symptoms, even to the point of death. Common approaches by athletes to deal with these very real nutritional issues include consuming sports drinks and/or solid electrolyte supplementation (capsules). The following table illustrates the function of critical electrolytes and provides a target dose during fluid intake and overall daily intake range for active individuals.

Both fluid and electrolyte intake are necessary during longer training and racing, depending on the athlete and conditions. To reiterate, for shorter efforts of two hours or less, most athletes do not need any form of fluid or electrolyte supplementation. Dehydration will set in and your electrolyte levels will rise, but in most cases will remain within a normal range. For efforts longer than about 2 hours, evidence would suggest that an athlete engaging in reasonable ingestion of fluid and electrolytes would attenuate the loss to a point where neither dehydration nor over-hydration would take place, and that electrolyte levels would remain within a normal range. "Reasonable ingestion" will depend on the losses specific to the athlete under the particular conditions.
With a nod to Dr. Noakes and his extensive research on the issue of over-hydration (summarized in his book Waterlogged), it was reported that "Athletes should drink to thirst during the race and not more than 800 mL/h," in the context of marathon running. On the subject of sodium intake, it was reported that during very prolonged exercise (such as an Ironman) that an acute sodium deficit may contribute to exertional hyponatremia. Our opinions differ on this point. As I illustrated in the model above, deficit can occur as soon as just a few hours, as well as by significant personal experience of sodium loss. Our bodies have finite reserves of sodium. A 70 kg (154 lb) human male contains a total of 100 g sodium (Human Body Composition, Volume 918, Steven Heymsfield) of which only 68 g is present in soft tissue (slow, but achievable exchange with plasma), including 10 g in blood.
What does this mean for an athlete losing 0.92 g of sodium in 1 L of sweat? It means that a meaningful deficit will occur with sufficient loss over time and without replacement. Dr. Noakes brings up a considerable body of evidence of over-drinking to support the position that most hyponatremia is induced by consuming more fluid than necessary. Indeed, the above model supports this as well, for example after 4 hours with 100% water replacement, hyponatremia is demonstrated. The model also supports the need for "reasonable intake" of fluid and electrolytes to slow the loss of both and to provide the athlete with a longer time window in which to sustain a given effort.
Dr. Noakes and I disagree on the need for any sodium replacement, and his book and papers go to great lengths to implicate the sports drink industry, and what he considers its questionable research and conclusions. If Dr. Noakes's criticism of the industry extends to supplements, I also have a product to sell (SaltStick). He brings up many relevant points and presents some interesting perspectives. However as with many scientific topics where experts disagree, there is no agreed-upon answer to the question of hydration and intake. Often-quoted are the excessive daily salt intake (10-15 g) of "western diets". My diet? I've calculated my daily salt consumption at under 2 g per day through food alone. You do the math if I'm out training for 2, 4 or 6 hours a day.
What about the change in loss of sodium in sweat over time? That's been documented, for sure. "In response to a low-salt diet and daily exercise in the heat, the kidneys begin to reduce their salt output within 1 to 2 hours, whereas salt excretion in sweat begin to fall only after 8 to 24 hours and requires several days to achieve a maximum effect (Robinson, Nicholas et al. 1955, as reported in Waterlogged). So reduce your daily intake to allow your body to adjust, but if you have a higher intake, you'll need to maintain a higher intake during exercise to provide the support to which your body is habituated.
My advice? Strive for a lower-sodium diet, and supplement according to the needs of your body. Similar to the thirst mechanism to seek hydration, the body's mechanism to seek sodium (salty foods, etc…) especially during exercise, indicates a need for added sodium intake. On the other hand, weight gain indicates too much intake of fluid and possibly sodium, and both should be restricted until body weight returns to normal or below normal.
Two competing factors, dehydration and hyponatremia, necessitate the balance between proper fluid intake and electrolyte intake. The key term here, "balance", means that there is an ideal athlete- and condition-specific plan to optimize performance and minimize health risks. Whether the supplementation is a solid electrolyte and water or a sports drink, long-distance athletes ignoring one or both of these aspects do so with the peril at best of limited performance, or at worst, at a danger to their health.
Jonathan Toker is a Canadian elite-level runner and triathlete. He received a Ph.D. in organic chemistry from The Scripps Research Institute in 2001, raced in the professional ranks as a triathlete for 5 years, and now mostly runs on trails. Dr. Toker worked as a scientist in the biotech industry for 5 years prior to launching his unique SaltStick Electrolyte Capsule and Dispenser lineup.

Start the discussion at slowtwitch.northend.network