How COVID Ripped Through a Hospital
It's all about triathlon. Except when it isn’t, and this is one of those Isn’ts. Below are excerpts from a thread on our Reader Forum, our off-topic forum we call the Lavender Room. They're written over a 6-week period, from a 20-year veteran of frontline work in intensive care medicine, and have been shared widely outside of Slowtwitch.
Our author's hospital is in the Washington DC area. The posts are about COVID patients. You’ll see a reference below to Dr. #2, and this doctor is from a hospital in another part of the country. I include his posts because the back-and-forth between them is highly instructional. Note how therapies are discussed several weeks before you and I first heard of them in the media.

March 31: "Most of you following the COVID threads know I work as a PA in critical care. Smallish community hospital on the border of DC/MD. Today the floodgates opened and we’ve been overrun with COVID patients. Here’s the quick snapshot of what that looks like … COVID patients in the ICU have doubled each of the last two days. It was a slow trickle at first, over the last two weeks. That phase is over. Game on.
"The staff, nursing and respiratory therapists in particular, are CONSTANTLY exposed to these patients, far more than the PAs or MDs. And they’re terrified. These are critical care nurses who’ve been there and done that. When COVID patients on vents—presuming they’re available—start hitting the other units, the nurses will be overwhelmed. This is coming, and it’s going to be ugly. I’m staying here overnight again to help out, and working the noon shift tomorrow."
April 2: "I just extended my run of four shifts to a run of nine and I’ll be sleeping here at the hospital more often than not. We’re trying to find the right balance of shifts to keep everyone healthy and sane, but it isn’t easy … At around 7pm tonight we deployed our last ventilator.
"Additional patients will be vented using anesthesia’s vents, which few of our RTs are familiar with from a practical management standpoint. There will be a learning curve. Plan C is to use the BIPAP machines as ventilators, though I have no idea how that will work.
"Our SICU unit is now fully COVID, 16 beds. 14 are on vents. None have come off yet, two have died. All still receiving the chloroquine-azithromycin-zinc cocktail. We still don’t really have an idea of the efficacy, but we’re sticking with it for lack of better options … Our ICU now has 9 COVID positive or rule-out (test results pending, treated like COVID+) and no fixed date for when our in house same-day results testing will be up and running. We’re just presuming at this point it isn’t going to happen.
"Nurses are getting crushed.
"I got off work last night at 11, home around midnight, and I drank bourbon alone until 3am when my brain finally let me sleep. I woke up at 7 to prepare for today’s shift."
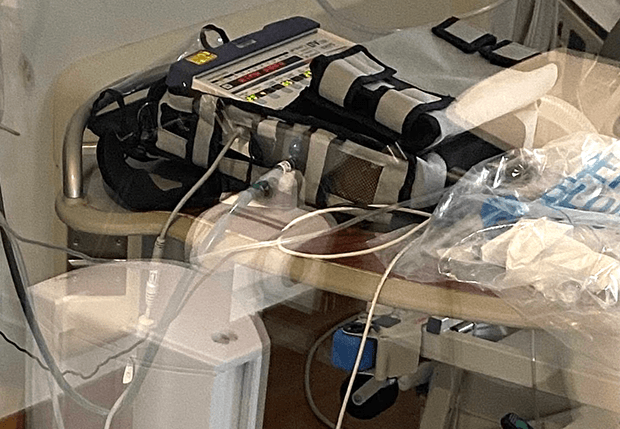
[PHOTO: Below is a typical infusion load for intubated COVID patients: blood pressure support, IV fluids, analgesia, sedation, paralytic, antibiotic infusion, etc. Pumps have been moved to the hallway so adjustments and changes can be made while minimizing exposure.]

April 3: "Gearing up for the 0700 shift now. I slept here in the call room last night, slept for five or so hours so I’m good for the day. Night shift had a rough one. Two more died of respiratory failure, both under 45. I think he said the last one was a 33-year-old woman, also previously healthy. X-Ray showed total white-out of both lungs …. Today we’ll be operating beyond our standard vent capacity for the first time, probably ever, so it should be interesting to see how things look by shift change tonight.
"We’re running out of sedation for these vented patients as well, now. Fentanyl is almost gone, benzos too—Versed, Lorazepam, Propofol, Precedex, everything getting very low according to my pharmacist. We’re switching to Ketamine drips which isn’t a bad choice, just somewhat unconventional."
April 4: "Yesterday was rough for the first 8 of 12 hours. One after another after another. Five intubations in the ICU alone. I was working solo with a man who transferred down from the IMC, who was admitted with suspected COVID two days prior. He's got no prior medical history, early 50s, lives with his wife who is now in another hospital with COVID infection confirmed. He went from 2L oxygen to a nonrebreather mask to intubated within a matter of hours. I intubated him in our unit, then let the RN loose to help out with other crashing patients. It's been a while since I've seen a guy get this sick so quickly, and it was disturbing. Drenched in sweat, frothing from the mouth like what you hear about rabies, heart rate in the 150s, and fighting like you wouldn't believe despite max dose Propofol (the "milk of amnesia" that killed Michael Jackson), 14mg of Versed, and 50mcg of Fentanyl.
"I let the nurse go (I had been keeping them outside the door since their PPE isn't up to our level, which is pretty shitty) when I started my procedures—arterial catheter and central venous catheter insertion—because I can manage the logistics myself and they don't need unnecessary exposure. I'm suturing the catheter into his neck, which is the final step of the CVC insertion, and he went ballistic. He's about 5-feet nothing, but fought like a raging bull. I had to lay my whole body weight across his chest to keep him from reaching up and ripping his tube and the catheter inserted in his jugular vein out, while suturing with my right hand and yelling for someone to come in and assist. I was able to finish suturing before anyone arrived (two simple knots) but the minute I got up he was swinging and bucking, red-faced, frothing, drenching sweat, just awful. I have never seen someone fight like that short of PCP intoxication. One of our docs, cross trained ICU-anesthesia, said he's seeing this pattern emerge with COVID patients, that they fight like hell through heavy sedation (not helping our shortage of sedation situation) and often require paralysis. Which is what I had to do the minute help arrived. I gave him an IV push of Norcuron, which gave us roughly 30 minutes of total paralysis to get him situated and properly sedated, restrained, and vitals under control. He was on 100% oxygen and 15 PEEP when I left, essentially maximum vent support, which is also typical now of COVID patients."

April 5: "This is, I hope, a generational event unlike anything I've seen in 20 years of medicine. This is NOT the flu. I just intubated patient number 6 of the day, a woman whose husband tested positive a few days ago. She went from 100% saturation on an oxygen mask, sleeping comfortable, to gasping for air and crying out for help in a matter of maybe 30 minutes. Saturations dropped to the mid-70s, heart rate spiked to the 160s, BP skyrocketed, and she just kept crying out "Help me, help me!" over and over. I've seen some shit in this business, but this is truly terrifying, on the deep end of these infections. They just crash SO FAST and hard, and we've yet to get one of these people off the ventilator. Last ballpark count was ICU, SICU both full, overflowing into PACU and now half of IMC is COVID, 90% on ventilators.
"I saw a patient first thing this morning and didn't recognize the ventilator, some toaster-sized device with minimal management capability. The respiratory therapist walked in, looked at it for a minute and said nothing. I asked if he knew where it came from or how to work it. 'I don't know what the fuck that thing is, but I'll figure it out…'"
[PHOTO: The ventilator below is roughly the size of a stereo system receiver, and has limited function. These are the bandaid, emergency vents you've heard about. They're now being used as primary ventilators, but it's still better than no vent at all if you absolutely need one.]
"The latest on the medical side is this. We're finding out in postmortem analysis that many, a statistically significant amount of deceased COVID victims specifically developed coagulopathy, resulting in DVT, PE, microemboli, and all sorts of downstream problems (kidney injury in particular), and so there's a real push to anticoagulate COVID patients to prevent these problems.
"Everyone who can be proned—turned to sleep or lay on their stomach—is being proned to recruit areas of lungs that tend to get gummed up with fluids and gunk when the lungs are injured. Very promising results with that, but again, the earlier the better, so proning someone on a vent is probably too late to make a meaningful difference.
"My brother has COVID, isolating himself at home, with 102 temp, myalgias, and persistent dry cough."
[PHOTO: Below is the entrance ramp to the main ICU. There are typically 2 dozen people waiting outside at any given time. The hospital implemented a zero visitor policy when things ramped up. The eerie quiet outside stands in stark contrast to what goes on inside.]

[On April 8th a doctor on the Reader Forum, working in a hospital in another part of the country, chimed in, and the two had a back-and-forth on what strategies yield success and failure.]
Dr. #2: "…not sure of the actual total number of healthcare givers, but the data says there are '32 colleagues/caregivers' COVID positive and 14 presently isolating at home…hope we don't run out of troops … 34 cumulative COVID deaths and 41 on vents presently with 81 COVID + in house, BUT 10 have come off vents and 83 COVID + have been discharged home. Yea!"
Our Author: "I've been off since yesterday morning but I've yet to extubate a COVID patient. I'm wracking my brain trying to synthesize all of the data coming out and I'm afraid we're keeping our patients too far to the dry side, exacerbating their hemodynamic instability and acute renal failure situation, going after this thing like we would ARDS with fluid overload."
Dr. #2: "I think one of the real tricks is to walk the wet/dry line as best as possible. Initially there was a lot of worry of ARDS-like capillary leak and bleeding, but I think the bleeding is from microvascular issues and cytokine storm late in the game. Worsening perfusion to the kidneys (*and other organs) leads to renal failure and gets them off the vent and onto dialysis and all that entails … I think erring on the dry side initially and once the lungs are stable (relatively), shoot for slight fluid positivity. If an U/S shows RV issues, they need volume, for sure, at that point.
"Read through the protocols I posted, if you haven't already seen them. It may help a bit, but this falls within 'the art of medicine.'"
Our Author: "My presumption was that RV issues (we're talking cor pulmonale?) result from higher PA pressures resulting from microemboli and thrombosis in COVID patients, but that wouldn't make physiologic sense. RV strain typically only occurs with massive PE burden, not micro pulmonary infarcts, unless shunting to an extreme degree develops.
"I feel naked managing these patients. There's just so much we don't know for certain, and we're literally watching people die as we try to figure it out."
Dr. #2: "I think any sign of RV strain, or underfilling of the LV, low CVP or any sign that is c/w hypovolemia goes along with a need for volume-in this case, as long as the lungs don't seem to be exhibiting issues with oxygenation. Remember, they are trying to avoid echo for COVID patients in general to reduce the risk to echo techs. And this is just my opinion-take it for what it's worth … There is no data or definitive guidelines, so we all have to do our best … and yes, people will die, but hopefully fewer as we get collectively better at this.
"You are doing great. Stay calm, stay confident and know you are doing all you can.
"I believe in you."
[PHOTO: Unrecognizable bodies in PPE suits, IV pumps, crash carts, central line carts, computers, x-ray machines, etc. These hallways are typically clear, with the exception of computer work stations.]

April 10: "My shift starts in a few minutes so I have our service's census data in front of me. Mean age is 61.3… We're two weeks in and have yet to successfully extubate a COVID patient. The patients who do best are the ones who never get intubated. I don't think the obvious conclusion holds anymore, that they do poorly on the vent because they were sicker than those who didn't require it in the first place. High flow oxygen, a higher threshold for intubation, mucolytics, bronchodilators, steroids, chest physiotherapy, and staying off the vent until pending respiratory failure might be the best chance for survival."
Dr. #2: "I reviewed the inpatient census on several of our hospital COVID floors of the vented patients with the ICU teams/pa's and others-most are:
Black
Hispanic
Obese
Hypertensive
Diabetic
Concominant heart disease
HX of cancer
Kind of in that order….
"But… a bunch more got off the vent in the past few days; many of the PA's I talked to today were very tired. A few patients in the MICU crashed last night needing intubations almost at the same time. Challenging times."
April 11: "Good news on this end, finally. We successfully extubated two COVID patients today, one to nasal canula, the other to high flow, but both looked solid at evening rounds. We also discharged the first COVID patient on our service, who never required intubation… I got off shift at 11pm, my 13th in 15 days, 12+ hour shifts, and I'm spent. Have to wake up early to hide easter eggs, but I'm sitting here at 1:46am drinking a bottle of wine because I can't unwind… I told my wife yesterday (we're going through divorce, to top it off) that I'm pretty sure I'm going to have some adjustment issues when this epidemic washes out. I've been dealing with the loss of a marriage, separation from my kids, and the stress of the ICU for about two years now, and now, the world's in crisis, where I've been for what feels like forever, so I feel normal again, if that makes sense."
April 16: "There are well over 100 confirmed COVID patients in our hospital … we are participating in the Remdesivir trial, which I believe started here three days ago. We can only hope. Nothing in the emerging data points to chloroquine being anything like the wonder drug It was touted as from the White House. Thankfully most people don’t look to that office for medical advice or reliable information in general, anymore.
"We are down to our last few ventilators. We’re using backup backup vents now, and they’re not great. We’ve had two fail in catastrophic ways which don’t need to be discussed further.
"I spent the majority of my time today with non-intubated COVID patients going into acute respiratory failure. Endotracheal tubes generally prevent the spread of droplets, so those are the safest patients to treat. Those just shy of needing a ventilator are the most dangerous to spend time with because they’re spewing droplets constantly with every labored breath. Today was the first day I felt actual fear for my health. Our entire IV therapy teams is out with COVID symptoms, and two of our SICU nurses.
"Our successful extubations are still celebrated, however they’re not keeping pace with terminal extubations, withdrawal of care, and death while providing care. This was anticipated, but still demoralizing. There are so many sad stories and developments happening here, it can be soul crushing if you let it. I think I mentioned that a mother and adult son are both COVID positive, in critical condition, in adjacent rooms… Mom may be extubated tomorrow as her RSBI and other parameters look promising. But she’ll wake up to learn that her son suffered cardiac arrest and a 20 minute resuscitation, now encephalopathic from anoxic brain injury, and will likely never open his eyes again.
"My shifts now begin at 9am and end after evening rounds, so with 70 or so patients, it often runs until midnight. I’m working tomorrow and sleeping here again tonight to cut down on the driving, and to be available if the pager goes off and the team is under water."
Dr. #2: "Sounds like your hospital is right at the brink, not too unlike mine. Our update today notes that we have 35 vents available still (and 47 patients on vents), but that is a somewhat artificial number given by the administration and includes promised vents from the gov't (not actually on hand). It also includes the crappy backup vents. In reality, we have 4… Did you see that there are a few small studies now suggesting steroids? We'll see what other things come out. I'm still curious about anti-coagulation."
April 21: "Tonight was a big development in our CC group meeting, though. Everyone explicitly acknowledged that we know enough now to stop using chloroquine, and to stick with Rem trials for those who qualify, daily steroids for everyone (it's an inflammatory process ultimately), proning, permissive mild hypoxia, and treating with supportive care primarily, and addressing any superimposing condition (bacterial pneumonia, flu, etc.) with standard medical therapies. I think it's the safest, smartest approach at this point. Vent management strategies are still a point of contention. We're using lower tidal volumes (6-7cc/kg.IBW) and very high PEEP. Results are mixed, and I think individualized approaches makes sense."
April 22: "We’ve had 5 COVID patients go into cardiac arrest today. Two were not critical care patients who died suddenly and unexpectedly, on low level oxygen. Three were in the unit. Two have survived to this point; one is in profound renal failure requiring hemodialysis and will not do well. The other was downgraded from ICU three days ago and was in good spirits and planning for discharge. That was a hard conversation with his wife ten minutes ago."
April 24: "Now it's hitting home. One of our group's intensivists, who's been meticulous about hygiene and PPE since COVID erupted here, tested positive day before yesterday, and is now being admitted to our hospital due to respiratory problems and persistent high fever. He's a very young 50-something with a history of bad asthma, otherwise healthy as a horse."
Dr. #2: "Today’s update said 60+ vents in use (new high) 122 cumulative COVID deaths (new high) and 84 colleagues COVID +. With another 29 at home isolating … ICU/extended units full of COVID patients and over 1/3 of hospital COVID +. Gowns running low…masks low…no end in sight with a much longer and flatter curve."
May 4: "The surge has definitely slowed, but our units are still consumed by it. We're still losing far too many people, relative to other common ICU illnesses like flu, sepsis, etc. We've run out of PPE gowns, though, which is problematic. The risk of transmission via contamination is, I think it's safe to say, unacceptably high now. But on that front, our ICU doc was discharged yesterday to a crowd of cheering staff clapping him out to the parking lot. It was a much needed moment of relief and release. It was very touching.
"I think at this point we've all adjusted to the grim reality of COVID in ICU patients. There's just so much suffering and dying. Yesterday I was inserting an arterial line on a COVID+ woman, with her dead fetus in the bed beside her. She developed COVID pneumonia and sepsis, and spontaneously aborted in the ER before she came up. It was awful. And then immediately after that we were cheering for our recovered doc. That's sort of how it goes up here, yo-yoing back and forth from one extreme emotional state to another."
May 8: "I don't know or pay attention to the numbers beyond our walls, but the internal data yesterday was pretty sobering. In our unit, in the month of April, we had 57 patients die on the vent, or withdrawn from vent support, versus 7 who were successfully weaned and presumably recovered. I rarely follow them after downgrade, presuming they've recovered, so I don't know the precise number beyond the fact of one of our vent-weaned patients ending up on a vent at a nearby hospital after discharge; so many non-ICU patients experienced sudden death on the low acuity wards and never made it to the vent, so I'm certain that our April number of COVID fatalities are 70+. That's an abysmal survival rate for critical patients, somewhere in the 13% range. It's fucking demoralizing, actually. I had three days off scheduled and now I'm working 2 of those three because a colleague got sick. Not unexpected, but damn it still sucks. We'll do mother's day when I get home Sunday morning."




Start the discussion at slowtwitch.northend.network