My Ablation
About 8 months ago I got an ablation for atrial fibrillation (afib for short). I’m been in sinus rhythm (normal heart rhythm) pretty much continuously since the procedure. No more afib since the ablation. Not wanting to perform an end zone dance prematurely I thought I’d wait until I was completely recovered from the procedure and that’s why I’m writing about this now.
Our cohort – lifelong hard charging endurance athletes – have an exaggerated incidence of afib. There have been to my knowledge 3 meta-analyses that report up to a 5-fold increase in afib for lifelong ardent endurance athletes compared to the general population. But that takes some explaining. Your chance of descending into afib actually goes down with moderate exercise, and more exercise further lowers your risk… until you start exercising like we do. It’s a U-shaped curve and when you get to the extreme edge of endurance effort the incidence of afib begins to rise sharply.
The Harder they come, the harder they fall, one and all
Fifty-two thousand Swedish nordic skiers competing in the Vasaloppet were studied years after they raced (it took about 10 editions of the race to accumulate that number of skiers). “Among male participants of a 90 km cross-country skiing event, a faster finishing time and a high number of completed races were associated with higher risk of arrhythmias.” That’s a good snapshot. The more we do it and the better we do it the more likely afib awaits us.
Men in particular continue to outpace non-athletes in afib incidence until later in life, when the ravages of an unhealthful life cause the general population’s rate of afib to catch up. It’s those middle years – when we’re in our 50s, plus or minus – that afib is a familiar diagnosis for us.
My first introduction to afib was at age-50, when I spent about 40 hours out of sinus rhythm (which is the term for a normal heart rhythm). I pretty much knew what was going on inside me as I drove myself to the emergency room. I “cardioverted” naturally, which is to say I did not get zapped back into sinus rhythm nor take anti-arrhythmic drugs. My heart just decided to beat normally again on its own.
Over the next 15 years I would fall into afib for several hours, or a day; it only happened once or twice a year; I would always cardiovert on my own; and I just accepted this as a way of life. Usually I overnighted in afib, arose, went outside for a gentle morning effort – such as a brisk dog walk for a mile or two – and my heart found its sinus rhythm before I returned home. Mind, that walk wasn’t 100 percent comfortable. Being in afib is no problem if you’re sitting, laying, doing nothing in particular. But try to run, or walk up stairs, and you feel as if you’re performing this act at 18,000 feet above sea level. Afib is not life threatening; it’s just very annoying and a great inconvenience unless your daily life consists of sleeping and the TV.
The Search for my doctor
At age-64 my afib got more frequent and each episode lasted longer. This is a typical progression. My longest stretch in afib was about 5 days. I then decided to begin the long process toward getting an ablation, which began with a search for the right doctor who’d perform the procedure. I found my doctor just through working the internet, looking for likely medical groups that I considered worthy candidates, and asking the doctors who I trusted for recommendations.
Cardiologists are either plumbers or electricians and a cardiology medical group will contain both specialties. UCLA Health (which includes UCLA Medical Center) has a cardiology department and I thought I’d found my electrician, and this cardiac specialty is called an electrophysiologist (EP). A good friend of mine – a lifelong high-caliber runner turned cyclist – had a successful ablation performed in another state. I asked my friend’s EP, “If you were to get an ablation for afib in the greater Los Angeles area who would you choose?” He came back with one name, no equivocating, a cardiologist at UCLA Health, but not the one I’d chosen through my Googling. It turns out there is – or can be – an even deeper specialization. The EP I’d landed on specializes in ventricular arrhythmias; the EP recommended to me was his colleague who specializes in atrial arrhythmias. I’d found the EP who’d perform my ablation. Now what?
I have a pair of cardiologists, my electrician and my plumber, and the latter was in charge of the testing. The point of it all is to give your EP a rough guess as to your general heart health and its architecture. Fortunately, my heart had not been “remodeled” by my afib, which often happens to those who seek ablations after spending years or decades in persistent afib (where you’re out of sinus rhythm all the time). Mine was paroxysmal afib (you’re in and out). Paroxysmal is what most long term endurance athletes will contract. As my ablation approached, however, I spent as much time in afib as out.
Then came my time for getting the procedure scheduled and I was disappointed to learn my ablation date was almost 4 months out. I was to told begin blood thinners a month before the procedure. I asked if I could start taking blood thinners right away so that in case of a cancellation I could say, “put me in coach.” The answer was yes and I got lucky: A cancellation occurred and I got my ablation in early June instead of my late-August date.
What exactly is an ablation?
Essentially, your EP kills the misbehaving part of your heart that throws off your heart rhythm. It’s a very small part of your heart and your doctor knows exactly where it is. How does he know? Let’s talk about the cardio-pulmonary system as a prelude to telling you what my EP did.
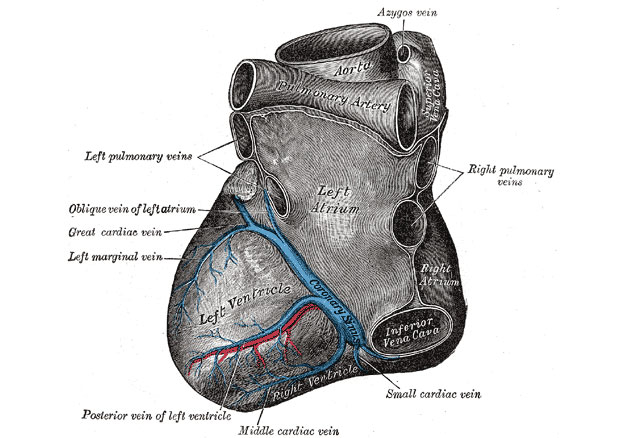
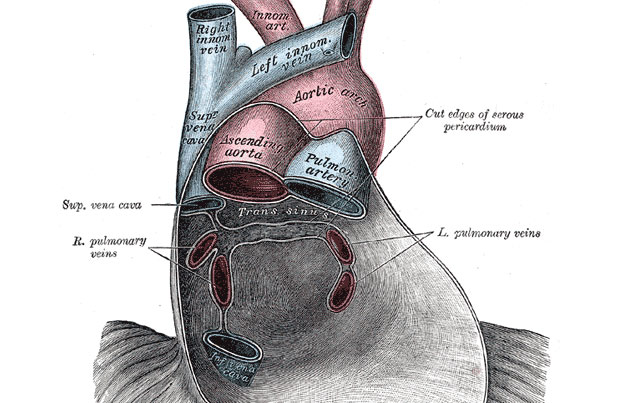
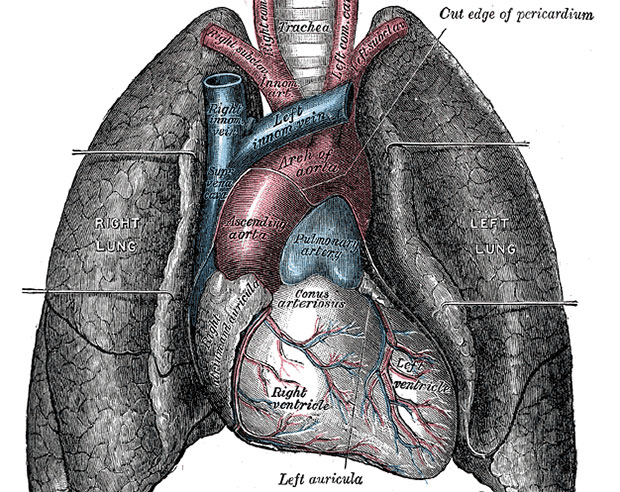
Veins take blood to your heart. Arteries take blood away from your heart. In general, that means arteries carry oxygenated blood, and veins carry deoxygenated blood but that’s not universally true. Deoxygenated blood makes its way into your heart through the superior and inferior vena cavae and remember, your heart has 4 chambers: 2 atria and 2 ventricles. Those two large veins enter into your right atrium, which delivers this blood into your right ventricle. The right ventricle contracts and delivers that blood to your lungs via the pulmonary arteries. (Yes, these are arteries because they’re leaving the heart, but the blood is oxygen-depleted.) The lungs are where that blood becomes oxygenated, and that O2-saturated blood returns to the heart via the pulmonary veins. (They’re veins because they’re making their way to the heart, but these veins contain oxygen-rich blood.) They enter the left atrium and right here is where the mischief occurs. Which I’ll come back to.
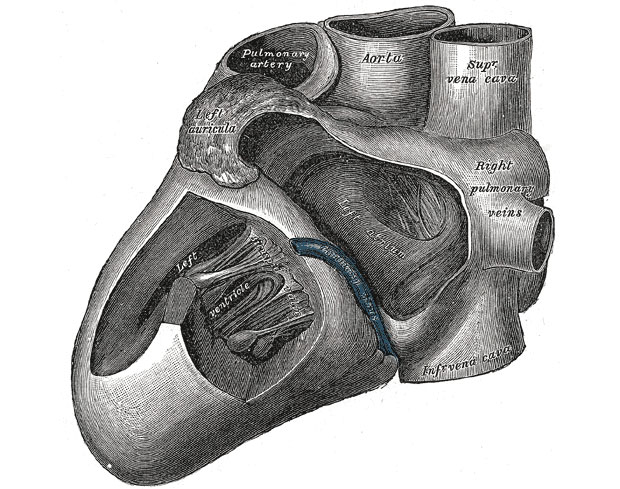
The left atrium collects your re-oxygenated blood, delivers it to the left ventricle, and BOOM, that’s the big enchilada. That’s the cannon shot delivering blood to your brain, organs, muscles and so on.
How does your EP know what or where to ablate?
Back to that left atrium. I don’t know why or how this happens but if I can channel the late Alan Greenspan there’s a kind of irrational exuberance in the heart tissue right at the point the pulmonary veins enter the left atrium (there are 4 veins that enter the left atrium, each of which brings oxygenated blood from the lungs to the heart). Where the vein enters the left atrium, this is the spot of the foul. While I have not asked my EP this question I believe he engaged in what is called Pulmonary Vein Isolation. Catheters are inserted into a blood vessel in the groin or in the neck, and those catheters are either diagnostic or they carry ordnance for the purpose of the ablation. The weaponized catheter cauterizes the area around the pulmonary vein using either heat or cold. Sometimes a balloon catheter is used, and these are inflated at the point of vein entry, enlarging the area to be ablated for (theoretically) a more precise procedure.
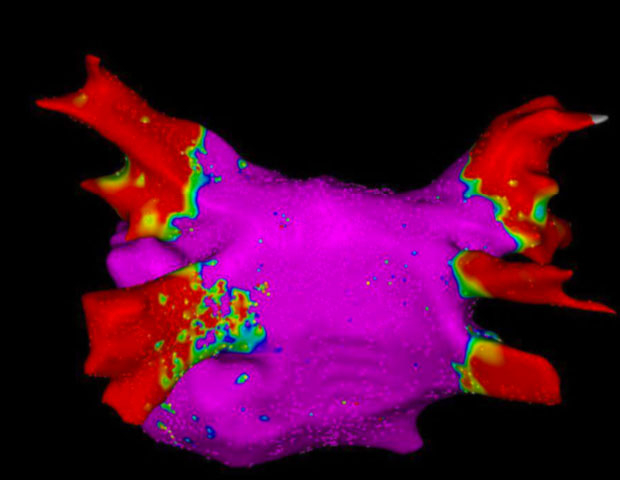
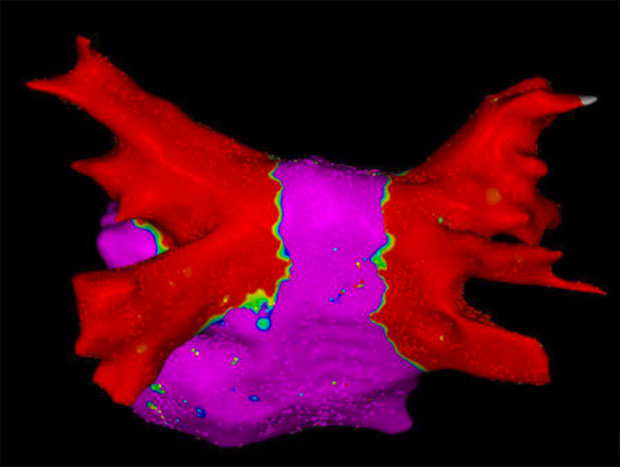
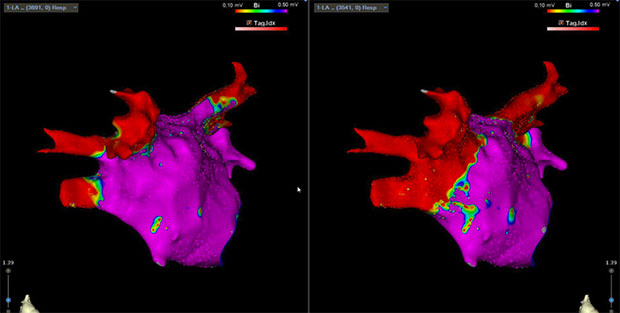
One helpful diagnostic tool is voltage mapping. Your EP can chart your heart’s misbehavior through looking at low-voltage areas that are color coded and I’m including the voltage map of my left atrium above that I believe is pre-ablation. If I understand it right, what you don’t want is yellow and green and that kind of doppler imaging that looks like a tornado is about to spring up. That nice, docile red area in the post-ablation image below is – as I understand it – a heart prepared to behave.
I asked my doc about what he ablated. The offending vein? Or all the veins? He said all of them because it was his experience (I believe in the neighborhood of 1,500 ablations) that if one was to ablate only the obviously misfiring vein it was a matter of time before the patient was back for another ablation of another pulmonary vein.
Recovery
I went for a swim session about a week after my ablation. Mistake. I really needed between 2 and 3 weeks before I was ready to resume anything like training. I found that my resting pulse was immediately 10 or more beats higher that usual, and that my max HR was a bit lower than it was pre-ablation.
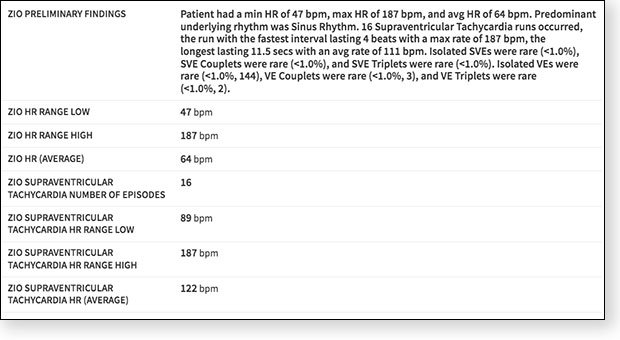
There’s a device called Zio patch that works like a holter, but it’s small in profile. It records a lot of data and a screenshot showing part of my Zio report is attached below, data from a 10-day stretch 4 months post-ablation. None of us are in sinus all the time and the Zio patch uncovered bouts of Supraventricular Tachycardia, with a max HR of 187 over a 4-beat stretch, and a max stretch of 11 beats @111bpm. I feel these "palpitations" occasionally but they’re minor. I more typically would go into afib – or experience a lot of pre-ventricular contractions (PVCs) – during a swim session. Bad sleep + lots of consecutive days of workouts + a hard swim session used to be a formula for afib. Now when I suspect I’m ripe for a bout of afib I remain – kind of to my surprise – in sinus.
I now am able to perform at my peak cardiac performance, or close to it. My resting pulse is now only a handful of beats higher than pre-ablation, and my ability to hit a high HR during a hard session is back. My FTP on the bike, and my capacity during the swim, has pretty much returned to where I was pre-ablation. I had a concern that my doctor killed too much in is zeal to prevent a reoccurrence, but that is not my experience. I swam the Ho’ala swim (the Kona swim course the week before Kona) in 1hr7min in 2019, and I swam it in 1hr8min in 2022 and that latter swim was exactly 4 months post-ablation. My Zio report came right after I returned from Kona, as you can’t have that device in the water and I wanted to wait until I could afford to take 10 days out of the pool.
I have no wisdom, exhortations, guidance, warnings, best practices to share. This just the “race report” of my ablation for those who wonder or will have cause to wonder what ablations for atrial fibrillation are all about. Yes there are triggers that pushed me into afib before my ablation and the major one was lack of sleep. But the big trigger was 50 years of a pretty high mileage, high heart rate lifestyle. Afib post-ablation might be analogous to cancer in remission: Your likelihood of a relapse is greater than if you never had it. I still might slip back into afib at some future date, or year, or decade. The best way to not experience heart arrhythmias is to throttle back your mileage and/or your effort. I’ll ponder the possibility of considering that, but I have a Zwift race in a few minutes I need to get ready for.
[LATE ADD: Since publication I've asked my EP and he gave me permission to disclose his name. He's Dr. Eric Buch (pronounced Bush) from UCLA Health in Los Angeles. Because the selection of the right EP was important to me I've placed a thread on our Reader Forum where readers can perhaps share, and inquire of, names of doctors in their areas that could be resources for those with atrial fibrillation.]




Start the discussion at slowtwitch.northend.network